What is cataract?
Maybe you think you’re just tired, but have you tried checking your blood sugar levels? If you haven’t gotten your bloodwork done in a while, you may want to check if you have diabetic retinopathy.
What is Diabetic Retinopathy?
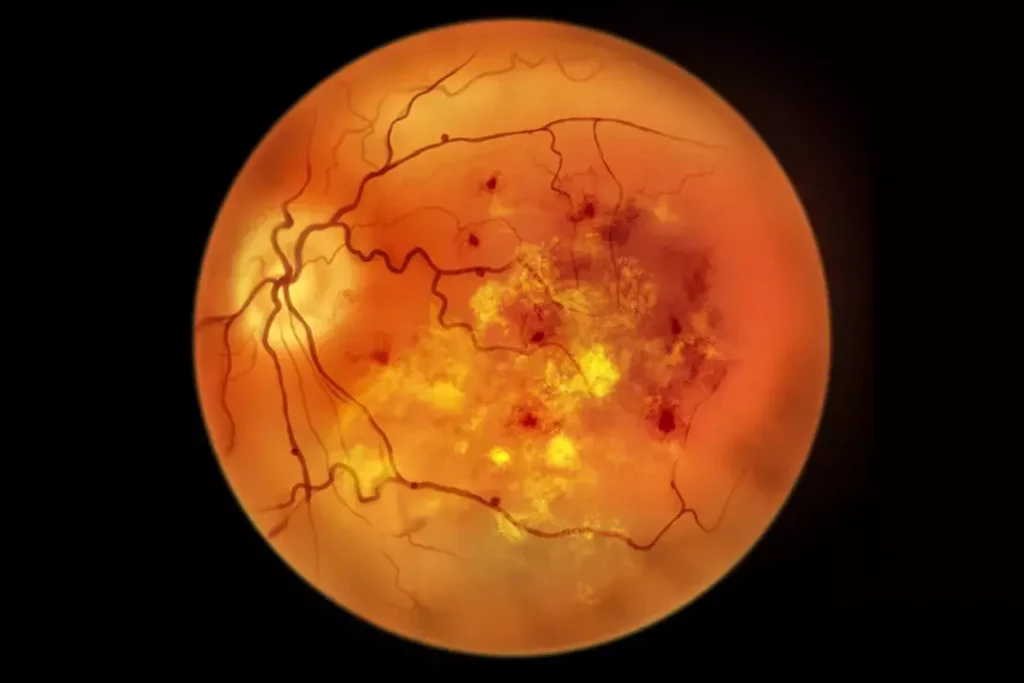
Diabetic Retinopathy (DR) is an eye condition secondary to diabetes. This happens when you have high blood sugar levels. Diabetic retinopathy can cause damage to the blood vessels in the retina, the light-sensitive tissue at the back of the eye. Raised blood sugar levels can cause damage to the retina, leading to loss of vision. This is why regular reviews with your GP to control blood sugar levels is essential in managing diabetic retinopathy.
Diabetic Retinopathy comes in two types: Non-Proliferative Diabetic Retinopathy (NPDR) or the early stage, and Proliferative Diabetic Retinopathy (PDR), also known as the advanced stage.
In early-stage NPDR, the blood vessels in your retina weaken and leak fluid or blood. This causes swelling (also called macular edema) or deposits (exudates). In the advanced stage (PDR), new blood vessels are growing on the surface of the retina or into the vitreous gel, which can bleed and cause vision loss.
How do I know if I have Diabetic Retinopathy?
The early stage of diabetic retinopathy does not come with obvious symptoms but as it progresses, the common symptoms include the following:
Blurred or distorted vision. When you have blurred vision, objects may appear out of focus or doubled while a distorted image appears bent or deformed.
Floaters (spots or dark strings) in the vision. Floaters may appear as ‘specks’ or ‘cobwebs’ in your vision. You may feel that your glasses always need cleaning! Floaters are often more noticeable when looking at a plain bright background.
Sudden loss of vision in one or both eyes. When you experience sudden loss of vision, this means your vision may suddenly darken or blur. You may even experience a complete blackout of the visual field in one or both eyes.
How do I know if I am at risk of getting Diabetic Retinopathy?
Certain cardiovascular risk factors may put you at risk of developing Diabetic Retinopathy such as having high and uncontrolled blood sugar levels, high blood pressure, high cholesterol levels, and gestational diabetes during pregnancy.
How is Diabetic Retinopathy diagnosed?
Getting a comprehensive eye examination is an effective way to diagnose Diabetic Retinopathy. These eye tests include visual acuity testing and optical coherence tomography (OCT) scans to assess the layers of the retina. Your Optometrist or Ophthalmologist may also instill dilating eye drops to assess the retina and optic nerve in detail.
Can Diabetic Retinopathy be treated?
What is Diabetic Macular Edema (DME)?
Another thing to watch out for is the risk of getting Diabetic Macular Edema or DME. DME is a specific complication of diabetic retinopathy that affects the central part of the retina responsible for sharp, central vision, which is the macula.
DME happens when fluid leaks into the macula, causing it to swell. This swelling disrupts the macula’s ability to function properly, leading to blurred or distorted central vision. This is caused by damage to the blood vessels in the retina due to having diabetes. If you have diabetes for a long time, it weakens the blood vessel walls, leaking the fluid into the surrounding retinal tissue, including the macula.
How to tell if I have Diabetic Macular Edema (DME)?
A blurred or distorted vision is most often reported by patients with DME. Some also experience seeing crooked lines, or washed-out or faded colors.
Am I at risk for Diabetic Macular Edema (DME)?
You may be at risk of getting the DME if you don’t control your diabetes; have diabetic retinopathy for a long while, high blood pressure and cholesterol levels, and being pregnant and diabetic.

